The United States is experiencing its worst measles outbreak in 33 years, a troubling setback in public health progress. As of early July 2025, at least 1,281 confirmed cases had been reported across 38 states and the District of Columbia, according to the Center for Outbreak Response Innovation (CORI) at Johns Hopkins University. This surge, the most severe since 1992, has already led to at least three deaths and more than 150 hospitalizations—most involving unvaccinated individuals.
The epicenter of the crisis is in Texas, particularly Gaines County, which accounts for 414 of the state’s 753 reported cases. While local authorities claim the spread in Gaines has been contained, transmission remains active in Lamar County, near the Oklahoma border. Even more concerning, the Texas Department of State Health Services recently confirmed two new cases unrelated to any known outbreaks, signaling ongoing community transmission.
Measles was officially declared eliminated in the United States in 2000, thanks to widespread vaccination efforts and rapid outbreak response. However, in recent years, growing vaccine hesitancy has eroded this achievement, leading to more frequent and widespread outbreaks.
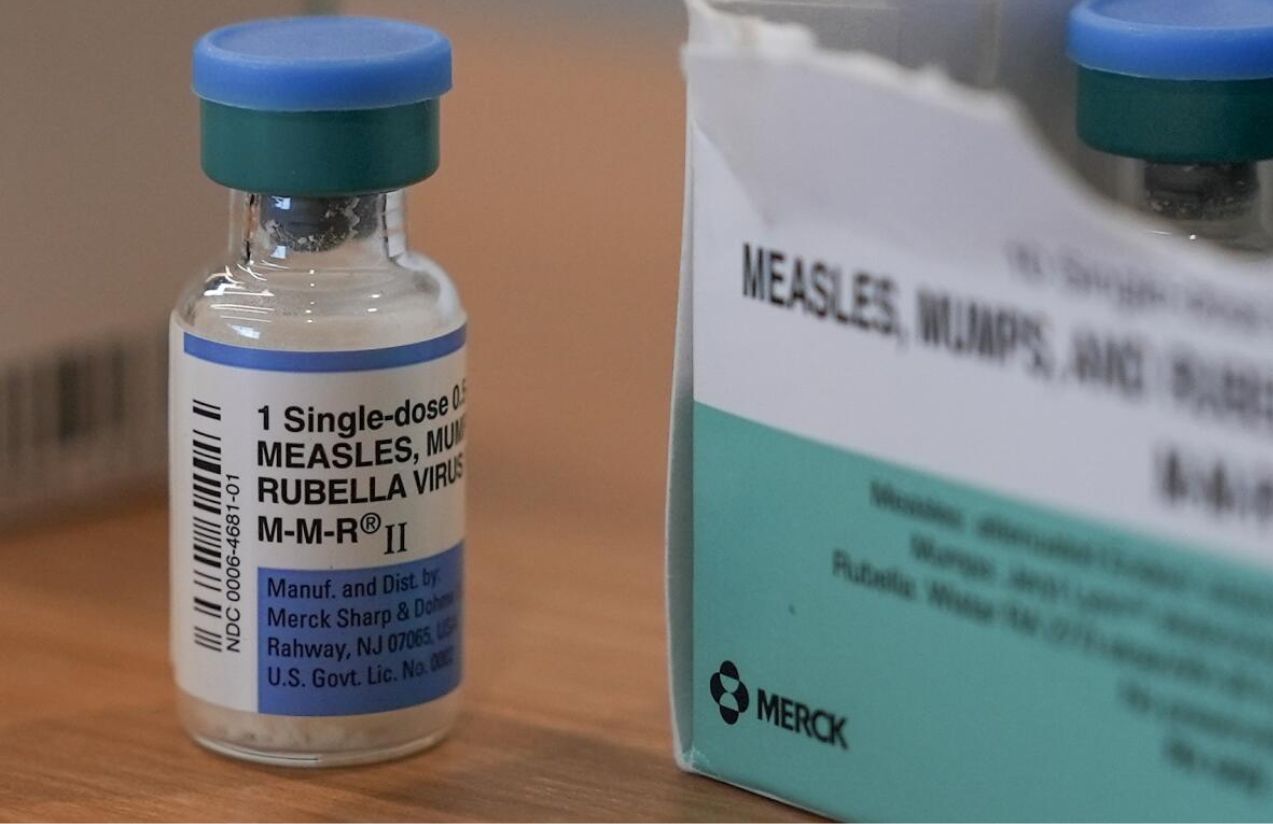
Health experts point to a key factor: the declining coverage of the MMR vaccine (measles, mumps, and rubella). In 2019, the national vaccination rate among kindergarteners was just above 95%—enough for herd immunity. Today, that number has dropped below 93% and continues to fall. In Gaines County, the rate is as low as 82%.
According to data from the Centers for Disease Control and Prevention (CDC), 92% of those infected in 2025 were either unvaccinated or had an unknown vaccination status. Among the hospitalized are two children from Texas and one man from New Mexico, none of whom had received the MMR vaccine.
The political response has sparked controversy. Health and Human Services Secretary Robert F. Kennedy Jr., a longtime vaccine skeptic, has sent mixed messages. While he officially supports vaccination, he has also amplified anti-vaccine rhetoric and promoted alternative treatments lacking scientific support. In June, he downplayed the initial Texas outbreak as “routine,” raising concerns among public health experts. Shortly after, he dismissed all 17 members of the CDC’s vaccine advisory committee and replaced them with prominent vaccine skeptics. The new committee has since announced plans to reassess the childhood vaccination schedule.
Further complicating the situation is the growing influence of anti-vaccine groups on social media, where many “health influencers” with financial incentives spread misinformation. Their messaging has even reached traditionally pro-vaccine communities, prompting some parents to vaccinate their older children while skipping immunizations for younger ones.
The current outbreak is already causing significant human and economic costs. For comparison, the 2019 outbreak in New York City—which was smaller than the one now unfolding in Texas—cost the city $8.4 billion and involved more than 550 personnel. Today, many public health agencies are struggling with limited resources due to federal funding cuts and tight post-pandemic budgets.
Texas has had to divert staff from other health initiatives to focus on measles containment. In Dallas County, 16 immunization workers were laid off due to budget cuts imposed by the Trump administration—even as the state faces its worst measles year in over three decades.
Despite the recent dip in new cases in Texas, public health officials like Philip Huang, director of Health and Human Services for Dallas County, warn the outbreak is far from over. They emphasize that unless vaccination rates rebound quickly, the U.S. risks losing its measles elimination status—an alarming shift that could reshape global public health benchmarks.